Abstract
Introduction: Numb Chin Syndrome (NCS) is a rare sensory neuropathy characterized by inferior alveolar or mental nerve damage. It manifests as hypoesthesia, paraesthesia, or pain in the chin and lower lip. Few case reports have been published on NCS secondary to sickle cell disease (SCD). As a result, information about causes, disease course and treatment are lacking. Our objective was to synthesize all currently available relevant literature on this rare condition.
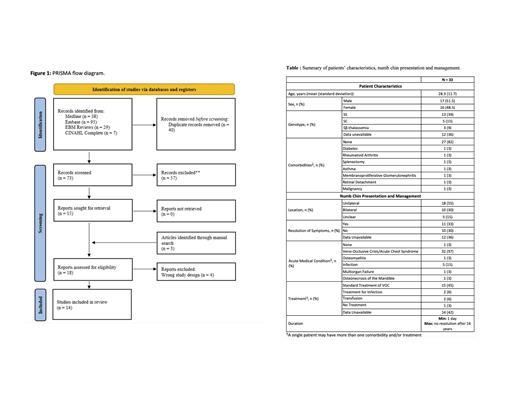
Methods: A systematic review was performed following the PRISMA guidelines. The following databases were searched: Medline, EMBASE and CINAHL Complete. The search strategy was designed by a librarian and utilized text words and relevant indexing terms to identify studies about NCS in patients with SCD. Conference abstracts of relevant scientific meetings were manually searched. No language limits were applied. Reviews, notes, editorials or comments were excluded. Patient demographics (including age, sex, country, SCD genotype), clinical presentation, investigations, treatment and outcomes were extracted by two independent reviewers.
Results: The systematic search revealed 73 publications (Figure). Only 11 publications from the databases and 3 from a manual search met the inclusion/exclusion criteria. Together, these case reports and series described 33 unique SCD patients. They originated from different regions (India, Turkey, Jamaica, USA, France, England). They were published between 1972 and 2021. Reports described between 1 and 13 patients each. Mean age was 28.3 years (standard deviation 11.7) and ranged from 11 to 60 years (Table). Sixteen were female. Genotype distribution was as follows: SS in 13 (39%), SC in 5 (15%), Sbeta-thalassemia in 3 (9%), not reported in 12 (36%). All but one case (97%) were associated with a vaso-occlusive crisis (VOC) and/or acute chest syndrome (ACS). One patient also developed multiorgan failure. One case occurred post dental surgery which led to a VOC. One case was associated with mandibular osteomyelitis and four others with infections. One patient presented with avascular osteonecrosis of the mandible. Comorbid medical conditions were reported as follows: rheumatoid arthritis treated with prednisone (1), pregnancy (1), type II diabetes (1) metastatic breast cancer treated by chemotherapy (1), membranoproliferative glomerulonephritis (1), asthma (1), retinal detachment (1) and splenectomy (1).
X-Rays were the most utilized imaging modality (10 [30%]), followed by CT-scan (7 [21%]), magnetic resonance imaging (MRI) (6 [18%]) and bone scan (2 [6%]). Two X-Rays revealed subtle radiolucencies suggestive of bone infarction, 1 X-Ray changes consistent with avascular necrosis and 1 X-Ray lytic lesions typical of osteomyelitis. One patient had a normal X-ray, but a CT-scan showed loss of cortical condensation around the mental canal which corresponded on a bone scan to a region of slightly increased tracer uptake suggestive of infarction. The MRI for one patient with bilateral NCS showed increased T2 signal in both mandibular rami with associated small subperiosteal fluid collections. One patient had a lumbar puncture that was normal.
Management of the neuropathy was mostly directed towards the underlying cause: treatment of VOC and SCD acute complications, antibiotics for infection, and tooth extraction for infectious control. Two patients received transfusions during their acute medical condition. The duration of symptoms ranged from a few hours to 14 years. Eleven patients (33%) were reported to have a complete resolution of NCS.
Conclusion: We provide a systematic review of the clinical manifestations, investigations and management of NCS in patients with SCD. NCS occurred most often in the context of VOC/ACS. Radiological evidence of mandibular infarction was reported for some. Together, this suggests that vaso-occlusion and bone infarction could be pathophysiological mechanisms of NCS. Careful evaluation is warranted to rule out differential causes including local infection, avascular necrosis, primary neoplasm or metastatic disease. Publication bias, a small sample size, and author-dependant lexical variability used to describe NCS are some limitations to our review. Through this largest report of NCS in SCD, we draw attention to a rare and potentially underrecognized neurological complication that deserves further investigation to optimize management.
Soulieres: Novartis: Research Funding; BMS: Membership on an entity's Board of Directors or advisory committees. Forte: Novartis: Honoraria; Canadian Hematology Society: Research Funding; Pfizer: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal